We are open for the receipt of specimens and the analysis of the majority of routine tests:
• From 09:00 to 18:30 Monday to Friday
• From 09.00 to 13.00 Saturday
Out of hours:
• Between 18:30 and 09:00 Monday to Friday
• 13:00 Saturday to 09:00 Monday
• Bank Holidays
During out of hour times, the laboratory is staffed by a single biomedical scientist to provide a service for emergency and essential hospital test requests.
The majority of routine tests have a turnaround time of 2 to 3 hours from the time of sample receipt. Providing a sample is received before 16.00, a result is normally available the same day.
We provide an urgent analysis service for a limited repertoire of tests if essential for the immediate management of a critical patient. We aim to have results available within 60 minutes of receipt of specimen.
During normal working hours (inc. Saturday morning and Bank Holidays):
Outside normal working hours:
NB. A telephone call is essential – failure to telephone the laboratory with details of the urgent request will result in samples being treated as category 3 samples, and will be accorded priority on the next scheduled batch and abnormal results telephoned as soon as they are authorised.
Forms marked with “please phone” are treated as category 3 samples. They are accorded priority on the next scheduled batch and results telephoned as soon as they are authorised.
Samples from ITU, ED AMU & NNU are automatically assigned category 1 status & treated as urgent.
DO NOT ABUSE THE EMERGENCY SERVICE; IT IS VERY COSTLY AND DEMANDING ON STAFF. IF THIS SERVICE IS USED INAPPROPRIATELY IT BECOMES SATURATED AND TURN AROUND TIME OF URGENT SAMPLES SIGNIFICANTLY INCREASES.
All routine samples can be podded to the laboratory, brought to the laboratory by the porters or can be brought directly to the laboratory and dropped off in person.
We welcome external referrals from any organisation, for any of our test repertoire. If you are a new requestor please complete the following form: New Requestor Form v3
We will process any sample referred to us meeting our sample labelling criteria.
Please Note: In line with the requirements of ISO15189:2012, each sample request will be considered a Service Level Agreement. To arrange a formal Service Level Agreement please contact the laboratory manager. Relevant Quality Statements for referred work can be found on the appropriate test page of this website.
We undertake to inform referring centres, without undue delay, in the event of circumstances that may adversely affect the reliability of results or turnaround times.
The laboratory requires the assistance of outside referral laboratories to perform analyses that the laboratory does not perform routinely, this may be for examinations or for consultant opinions. Deciding which laboratory to use is be based on numerous factors (e.g. expertise and skill, competency, references, cost, turnaround time, proficiency, proximity, accreditation status, EQA participation).
The Blood Sciences Laboratory is responsible for selecting the referral laboratories and takes steps to monitor the quality of performance and ensure that the referral laboratories are competent to perform the requested examinations. This is achieved by letter which is sent to all referral laboratories. A register of all the approved referral centres is kept for all the departments within the Blood Sciences Quality Management System, and this information is requested and updated annually.
Sample requests are triaged into 3 categories.
Category 1 – ‘STAT’ or ‘1 hour urgent’
These samples take priority over all other samples. These specimens are treated as genuinely urgent, and will be processed immediately on arrival. However, in order to process urgent samples, the requesting Doctor must follow the procedures as outlined in ‘Urgent requests above’.
Samples from specific wards: ITU, A&E, EMU, CDU, STAU, WYAC, MTU,PAU & NNU are automatically assigned category 1 status & treated as urgent.
Urgent request results are not usually telephoned, but are available on ward terminals within one hour. If results are abnormal, they fall within our telephone policy and are telephoned as soon as they are validated.
Category 2 – Waiting patient or ward staff.
Suitable only for short turnaround time tests.
A sample from a waiting patient or ward staff should be brought to the Blood Sciences laboratory and identified as a sample from staff or patient intent on waiting for the result. The sample is processed through the urgent system and undergoes immediate labelling, booking-in and centrifugation, then is taken to the appropriate section for analysis. An analyser print out is given to the person waiting.
Category 3 – ‘Three hour urgent’
Samples that are received with the urgent box marked, but no prior urgent telephone request had been made.
These samples are allocated to the routine reception area, but are given priority over other routine samples. The results are not telephoned unless they are abnormal and fall within our telephone policy. Results should be available on ward terminals within three hours.
Add on tests
If add-on tests are required, please note the following information:
Requests made from within the hospital:
Requests from Primary Care:
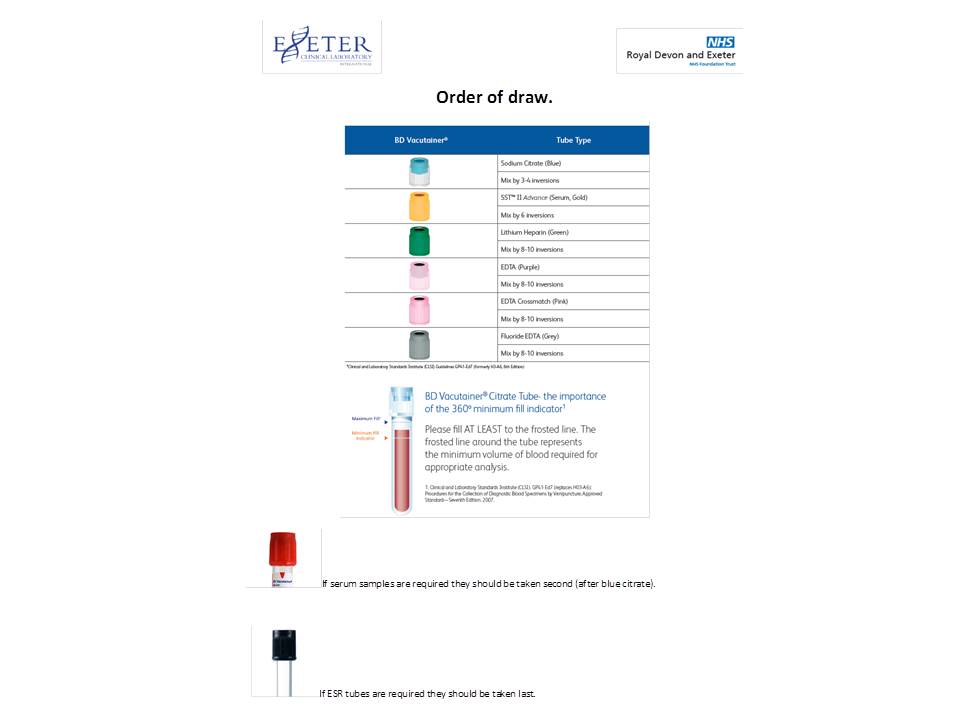
Order of Draw
Telephoned Results
Please note: Telephone limits changed on 5th August 2024. With the exception of specific local agreement, the new limits are aligned across Devon and Cornwall and are based on National Guidance from the Royal College of Pathologists.
Results falling outside of the limits below will be telephoned to the requestor or requesting location wherever possible. For GP requests every endeavour will be made to contact the surgery within working hours. Devon Doctors will be contacted out of working hours.
Telephone Limits from 5th August 2024
| Parameter | Lower limit | Upper limit |
| Chemistry | ||
|
Acute Kidney Injury flags All stage 3 flags All stage 2 flags to GP’s and RDE OPD patients All AKI 1/2/3 in children to requesting clinician or paediatric registrar |
||
|
AST (Adult Female) AST (Adult Male) AST (Under 18 years) |
500 IU/L or above 600 IU/L or above 500 IU/L or above |
|
|
ALT (Adult Female) ALT (Adult Male) ALT (Under 18 years) |
500 IU/L or above 600 IU/L or above 500 IU/L or above |
|
| Ammonia | 100 umol/L or above | |
|
Amylase (up to 15 days) Amylase (15 days up to 13 weeks) Amylase (13 weeks up to 1 year) Amylase (1 year and above) |
55 umol/L or above 125 umol/L or above 290 umol/L or above 500 umol/L or above |
|
| Bicarbonate | 10 mmol/L or below | |
| Bile Acids | 40.0 umol/L or above | |
| CSF glucose | 1.9 mmol/L or below | 6.1 mmol/L or above |
| Calcium (adjusted) | 1.80 mmol/L or below | 3.50 mmol/L or above |
| Carbamazepine | 21 mg/L or above | |
| Creatine kinase | 5000 IU/L or above | |
| Cortisol | 99 nmol/L or below | |
|
Creatinine (Adult non renal patient) Creatinine (Children less than 16 years) |
354 umol/L or above 200 umol/L or above |
|
| CRP (GP only) | 300 mg/L or above | |
| Digoxin | 2.5 ug/L or above | |
| Ethanol | 4000 mg/L or above | |
|
Glucose (Adult) Glucose (Children less than 16 years) |
2.5 mmol/L or below 2.5 mmol/L or below |
25.0 mmol/L or above 15.0 mmol/L or above |
| Gentamicin | 7.1 mg/L or above | |
| Glycated Haemoglobin (previously unknown diabetic only) | 121 mmol/mol or above | |
| Iron | 90.1 umol/L or above | |
| Lactate | 2.5 mmol/L or above | |
| Lithium | 1.50 mmol/L or above | |
| Magnesium | 0.40 mmol/L or below | |
| Bilirubin (Neonate) | Age/gestation specific treatment threshold | |
| Conjugated bilirubin (less than 60 days) | 25 umol/L or above | |
| Paracetamol | 30 mg/L or above | |
| Phenytoin | 25 mg/L or above | |
| Phosphate | 0.30 mmol/L or below | |
|
Potassium (primary care) Potassium (hospital) |
2.5 mmol/L or below 2.5 mmol/L or below |
6.1 mmol/L or above 6.5 mmol/L or above |
| Salicylate | 300 mg/L or above | |
|
Sodium (Adult) Sodium (Children less than 16 years) |
120 mmol/L or below 130 mmol/L or below |
160 mmol/L or above 160 mmol/L or above |
| Theophylline | 25 mg/L or above | |
| Troponin T (GP only) | 15 ng/L or above | |
| Urate (during pregnancy) | 340 umol/L or above | |
|
Urea (Adult non-renal patient) Urea (Children less than 16 years) |
|
30.0 mmol/L or above 10.0 mmol/L or above |
| Haematology | ||
| Haemoglobin | 70 g/L | |
| Haemoglobin (neonate) | 100 g/L | |
| INR | 6.5 | |
| APTR | 3.00 | |
| D Dimer (GP only, 50 years or less) | 230 ng/mL | |
| Platelets | 50 10*9/L | |